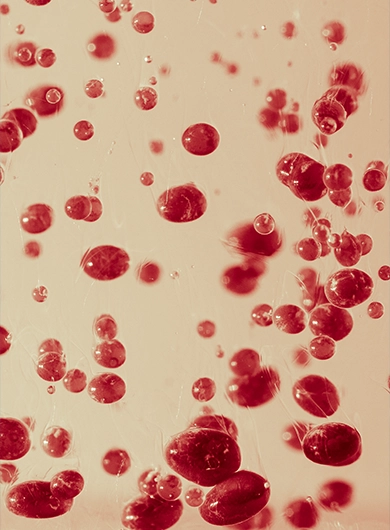
SVF Adipose Stem Cells
Our Team
We are a team of highly specialized spine surgeons dedicated to pioneering the future of spine care.
Share:
Table Of Contents
- Stromal Vascular Fraction (SVF): Advancing Regenerative Spine Care
- Origin and Composition of SVF
- How SVF Differs from Other Stem Cell Therapies
- How SVF Is Used in Regenerative Spine Treatments
- The SVF Procedure: What Patients Can Expect
- Clinical Benefits of SVF for Spine Health
- Is SVF Therapy Safe and Effective?
- Who’s a Candidate for SVF-Based Spine Care?
- SVF vs. Other Regenerative Therapies
- The Future of SVF in Regenerative Spine Medicine
- Frequently Asked Questions (FAQ's)
- External Sources
Stromal Vascular Fraction (SVF): Advancing Regenerative Spine Care
Introduction: Stromal Vascular Fraction (SVF) is revolutionizing regenerative spine care by providing a minimally invasive, biologically potent alternative to traditional surgical treatments. Derived from the patient’s own adipose tissue, SVF offers promising outcomes for those suffering from chronic back pain, disc degeneration, or herniated discs. In this guide, we’ll explore what SVF is, how it works in spine treatment, and why it may be the future of non-surgical spine recovery.
Origin and Composition of SVF
SVF is a cell-rich substance extracted from fat (adipose) tissue. It contains a powerful mix of mesenchymal stem cells, endothelial cells, growth factors, and cytokines, making it uniquely capable of promoting repair and regeneration.
How SVF Differs from Other Stem Cell Therapies
Unlike isolated stem cell injections, SVF is a complete biological product that includes a supportive microenvironment of regenerative components. This cellular synergy enhances its healing potential.
How SVF Is Used in Regenerative Spine Treatments
Application in Disc Degeneration, Herniated Discs, and Chronic Back Pain
SVF is injected directly into degenerated or damaged spinal discs to support tissue repair, reduce inflammation, and alleviate nerve compression symptoms.
Combining SVF with Minimally Invasive Spine Surgery
In some cases, SVF is used alongside endoscopic discectomy procedures to accelerate healing and reduce the risk of reherniation after disc removal.
The SVF Procedure: What Patients Can Expect
Adipose Tissue Collection and Processing
A small amount of fat is harvested, usually from the abdomen or thighs. The tissue is processed in a sterile lab to isolate the SVF.
Injection into the Targeted Spine Area
Under image guidance, the SVF is injected into the affected spinal region to begin the healing process.
Outpatient Process and Recovery Timeline
The entire procedure takes approximately 4 hours and is typically completed in an outpatient setting. Most patients resume normal activity within days.
Clinical Benefits of SVF for Spine Health
Promoting Natural Healing and Anti-Inflammatory Response
SVF’s high concentration of anti-inflammatory and regenerative cells helps reduce swelling, relieve pain, and stimulate the body’s natural repair mechanisms.
Reducing the Need for Traditional Surgery
By offering a biologic alternative, SVF may eliminate the need for invasive spinal surgeries in eligible patients.
Minimizing Reherniation Risk After Discectomy
Post-surgical reherniation can be mitigated by SVF’s ability to fortify spinal disc tissue and improve healing integrity.
Is SVF Therapy Safe and Effective?
Safety Profile Based on Current Studies
Multiple clinical trials support the safety of SVF. As the cells are autologous (from the patient), the risk of rejection or allergic reaction is minimal.
Common Side Effects and Patient Tolerance
Side effects are rare and typically limited to mild discomfort or swelling at the injection site. Most patients report high satisfaction.
Ongoing Clinical Trials and Regulatory Insights
SVF is still being studied in various spine-related applications. It is not FDA-approved for all uses, but many clinics offer it under IRB protocols or expanded access programs.
Who’s a Candidate for SVF-Based Spine Care?
Ideal Spine Conditions for SVF
- Mild to moderate disc degeneration
- Herniated discs without severe nerve damage
- Chronic back or neck pain not responding to traditional care
Contraindications and Limitations
Patients with active infections, uncontrolled diabetes, or recent cancer diagnoses may not be eligible. A thorough medical evaluation is required.
SVF vs. Other Regenerative Therapies
SVF vs. PRP and BMAC
While PRP and BMAC offer benefits, SVF provides a richer cellular mix and is believed to deliver stronger regenerative outcomes for spine conditions.
When to Use SVF as a Standalone or Adjunct
SVF can be used on its own or in combination with surgical procedures to improve recovery outcomes.
The Future of SVF in Regenerative Spine Medicine
Emerging Innovations
Advanced delivery systems, scaffold-enhanced applications, and gene-modified SVF may redefine spine care in the coming years.
Potential for Broader Spinal Applications
Research is expanding into SVF’s role in treating spinal stenosis, sciatica, and post-surgical healing.
Ready to explore SVF for spine healing?
Schedule an Appointment with Total Spine Wellness and discover if SVF therapy is right for your condition.
Frequently asked questions (faqs)
What is Stromal Vascular Fraction (SVF) used for in spine care?
SVF is used to promote disc regeneration, reduce inflammation, and support natural healing in spine conditions.
Is SVF therapy safe for spinal disc issues?
Yes. Clinical data suggests SVF therapy is generally safe and well-tolerated when administered properly.
How long does it take to recover from SVF therapy?
Most patients resume normal ctivity within a few days post-procedure, with ongoing improvement over weeks.
What’s the difference between SVF and stem cell injections?
SVF contains a broader range of regenerative cells and growth factors compared to isolated stem cells.
Who qualifies for SVF-based regenerative spine treatment?
Patients with mild to moderate disc issues, chronic back pain, or failed conservative treatments may qualify.